Guides, leaflets and resources
Vulval pain information
Do you have unexplained female genital pain?
If all tests for infections come back negative but you still experience discomfort, burning or soreness, you may have vulvodynia.
Unprovoked vulvodynia is characterised by continuous burning, stinging or soreness of the vulva.
Provoked vulvodynia (vestibulodynia) refers to pain experienced when pressure is applied to the vestibule (the entrance to the vagina) – for example, during sex or when inserting tampons.
Over a quarter of women will have vulvodynia at some point in their lives.* It can be distressing but treatment and support are available.
Vulvodynia
Vulvodynia is the term used to describe the sensation of vulval burning, soreness or pain in the absence of any obvious skin condition or infection. Symptoms may be constant (unprovoked vulvodynia) or only evident on touch (provoked vulvodynia, also referred to as vestibulodynia).
Diagnosis must be made by a doctor knowledgeable about vulval problems. If you think you may have vulvodynia ask your GP, or local Genitourinary Medicine (GUM) clinic, for a referral. Ideally, you should do this as soon as possible, since a delay in getting an accurate diagnosis and treatment could lead to the pain becoming much harder to treat successfully in the long term.
Some doctors may not be familiar with the condition. This leaflet provides information, support and advice for women with vulvodynia and members of the medical profession.
An illustration of the vulva, showing which areas may be affected
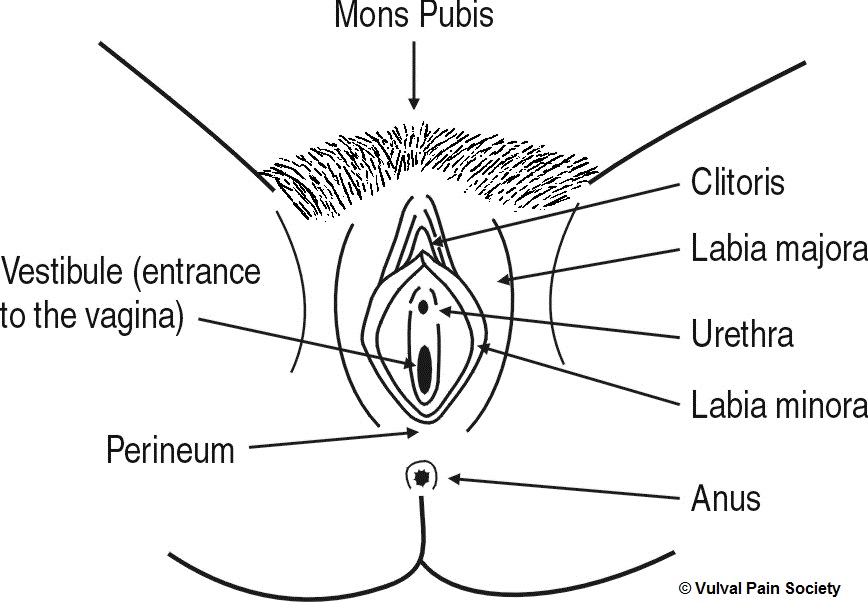
Explanation of the diagram
This is a black and white line diagram of the vulva. The vulva is viewed from the front, looking between the legs, with the woman lying on her back and the vulva spread open to show its inner parts.
Working from top to bottom of the diagram, so from the front to the back of the body, and from the outside inwards, the parts of the vulva shown are as follows:
- Mons pubis – the hairy, fatty triangular pad on the front of the body, just above the vulva
- Labia majora – the hairy, fatty outer lips containing the inner vulva
- Labia minora – the hairless, fatless inner lips inside and between the labia majora
- Clitoris – a pea-sized organ located at the top meeting point of the labia minora below the mons pubis
- Urethra – the opening used to pass urine, located between the labia minora, below the clitoris and above the vaginal opening
- Vestibule – the entrance to the vagina, located between the labia minora around the vaginal opening
- Perineum – the bridge of skin and muscle located at the bottom meeting point of the labia majora, between the vaginal opening and the anus
- Anus – the external opening to the bowel, located below and behind the perineum towards the back.
Unprovoked vulvodynia
What is it?
The condition is characterised by vulval burning and soreness, usually as a consequence of irritation or hypersensitivity of the nerve fibres in the vulval skin.
Symptoms are often constant and intensity may vary from mild discomfort to severe constant pain, which can interfere with sleep and sexual activity, and even prevent sitting or the wearing of trousers. Some women also experience related pain around the inside of the thighs, the upper legs and the anus. The burning sensation may be generalised over the entire genital area, or localised to just the clitoris (clitorodynia), or one side of the vulva only (hemivulvodynia). Itching is not generallly a feature of the condition.
Usually there is nothing to see on examination as the problem lies with the nerve fibres themselves, which are not visible to the naked eye.
For a minority of women with vulvodynia, back problems can cause spinal nerve compression and referred pain in the vulval area. In the majority of cases, however, the precise cause of the nerve damage, irritation or misfiring remains unknown.
How is it treated?
Pain that originates from nerve fibres is best treated with drugs that alter the way the nerve fibres send their impulses to the spinal cord and create the sensation of pain. Pain-modifying drugs such as tricyclic antidepressants act in this way and have been used extensively to treat vulvodynia. (Note that they are not prescribed to treat depression in this case, but to dampen down the pain signals travelling the nerves, and thus ‘retrain’ the nerves to function normally, i.e. without producing chronic vulval pain.) The drugs are available from your doctor and examples include amitriptyline, nortriptyline and dothiepin. Sometimes drugs such as gabapentin or pregabalin are also used in the treatment of vulvodynia.
Chronic pain strategies such as acupuncture, mindfulness and stress management may also help relieve symptoms. Bland emollient creams and vaginal lubricants may also be of benefit. See the Vulval Pain Society’s website (details given below) for more information.
Be wary of applying non-prescribed creams to the vulva as some can cause irritation.
Provoked vulvodynia (vestibulodynia)
What is it?
In 1987, American gynaecologist Edward Friedrich described a group of women who experienced severe pain and discomfort of the vestibule area at the entrance of the vagina.
The pain experienced by some women with vestibulodynia is variable; some are able to have penetrative sex, whilst others find that even light touch or wearing trousers can be excruciating.
Often on examination of the vestibule there is tenderness to light touch. There may be red areas at the site of tenderness, but frequently the findings are ‘normal’. Tests should be done to rule out infections and vulval skin conditions that may cause similar symptoms. Some doctors are unaware the condition exists and can often mistake it for thrush. Repeated use of topical anti-thrush treatments can make the condition worse.
It is likely that a number of factors cause vestibulodynia, but often no identifiable cause can be found. Some women have a sudden onset of symptoms following a specific event: commonly a severe attack of thrush followed by anti-thrush treatment, or after giving birth.
How is it treated?
Women with vestibulodynia often benefit when treatments are combined. These can include skin desensitisation (making skin less sensitive) through massage, pelvic floor muscle physiotherapy, psychosexual counselling, and rarely, surgery (vestibulectomy).
Associated vulval conditions
Lichen sclerosus, lichen planus, eczema, psoriasis
There are also a number of skin conditions that can affect the vulva – a few are listed above. They are usually characterised by itchiness; the skin may be red and inflamed, as in eczema, or white patches may be visible, as in lichen sclerosus. Initial treatment is usually with a steroid cream or ointment. Diagnosis needs to be made by a doctor.
Painful bladder syndrome (PBS)
PBS (formerly known as interstitial cystitis) refers to chronic symptoms of urinary urgency and frequency, pain and burning, in the absence of a bladder infection.
Some women with vulvodynia also experience bladder symptoms, and it is possible to present with more than one vulval condition simultaneously.
What unprovoked vulvodynia and vestibulodynia are NOT
They are not sexually transmitted infections and cannot be passed on to a partner. PBS and the skin conditions listed above are also non-infectious.
They are not forms of vaginismus (involuntary tightening of the vaginal muscles), though vaginismus can develop as a response to pain in the vagina or vulva.
They are real physical conditions and do not have a psychological cause. Psychological distress may develop as a consequence of ongoing pain or discomfort and in this instance women (and their partners) may benefit from seeing a psychosexual counsellor.
The Vulval Pain Society
The Vulval Pain Society is a UK registered charity, number 1118118, providing support and information to vulvodynia sufferers and their partners. It was set up in 1996 by gynaecologist Dr David Nunns and nurse Diane Hamdy.
Contacts
The Vulval Pain Society (VPS)
Post: VPS, PO Box 7804, Nottingham, NG3 5ZQ
UK Lichen Planus (UKLP)
Further information
Details of local support groups, workshops and treatment options can be found on the VPS website at
For printed copies of this leaflet free of charge, please email or write to the VPS at the address given above, or you can download a PDF copy using the link at the end of this article. You may freely photocopy or copy the leaflet in any of these formats provided authorship of VPS and LVPSG (the London Vulval Pain Support Group) is clearly acknowledged.
*Reed BD et al. Prevalence and demographic characteristics of vulvodynia in a population-based sample. Am J Obstet Gynecol. 2012 Feb;(206)2: 170.e1-170.e9.
Leaflet produced by the London Vulval Pain Support Group in association with the Vulval Pain Society. Copyright of Vulval Pain Society and London Vulval Pain Support Group 10 March 2018.
Last updated 14 November 2018