Vulval self-examination
Why vulval self-examination?
There are many conditions that affect the vulval skin such as infections, skin diseases e.g. lichen sclerosus, pre-cancerous cells and rarely, cancer. More and more women are visiting their doctors with these vulval conditions. The sooner treatment can be given, the less likely it is that you will suffer from symptoms and this may potentially reduce the extensiveness of treatment. The key is early detection.
What is the vulva?
This term refers to a woman’s external genital organs, which include the inner and outer ‘lips’ and clitoris.
Diagram of the vulva
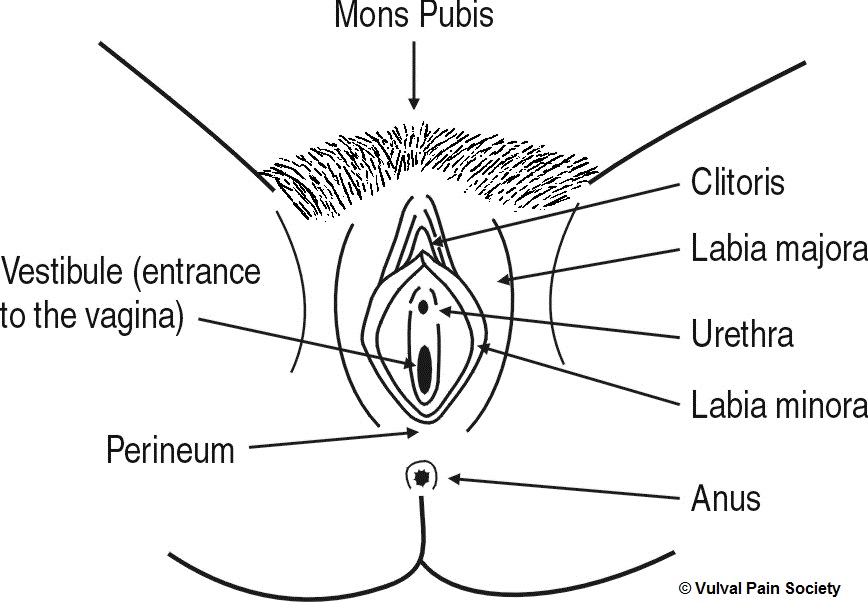
Explanation of the diagram
This is a black and white line diagram of the vulva. The vulva is viewed from the front, looking between the legs, with the woman lying on her back and the vulva spread open to show its inner parts. When performing self-examination using a mirror, this is the image seen in the mirror.
Working from top to bottom of the diagram, so from the front to the back of the body, and from the outside inwards, the parts of the vulva shown are as follows:
- Mons pubis – the hairy, fatty triangular pad on the front of the body, just above the vulva
- Labia majora – the hairy, fatty outer lips containing the inner vulva
- Labia minora – the hairless, fatless inner lips inside and between the labia majora
- Clitoris – a pea-sized organ located at the top meeting point of the labia minora below the mons pubis
- Urethra – the opening used to pass urine, located between the labia minora, below the clitoris and above the vaginal opening
- Vestibule – the entrance to the vagina, located between the labia minora around the vaginal opening
- Perineum – the bridge of skin and muscle located at the bottom meeting point of the labia majora, between the vaginal opening and the anus
- Anus – the external opening to the bowel, located below and behind the perineum towards the back.
How to perform vulval self-examination
Find a private place such as your bedroom and hold a mirror in one hand. Try and get a good view of the vulval area by separating the outer lips. The diagram above indicates the different parts of the vulva (external genitals) which should be examined individually. Each area can be both looked at and touched gently with a finger. Start at the top with the ‘mons pubis’ which is the area above the vulva around the pubic bone where the pubic hair is located. Then work down checking the clitoris, labia minora, labia majora, perineum (area between the vaginal opening and the anus) and finally the anus.
How often should vulval self-examination be performed?
Once a month in between periods or at any time when you develop vulval itching or pain, pain on penetration during sex, or when you feel vulval lumps or thickening of the skin.
Who should perform vulval self-examination?
Women who are sexually active and all women over the age of 20 years.
What should I look for?
Changes in the vulval skin. Some examples of changes include:
- Any changes in the colour of the vulval skin such as whitening or an increase in skin pigmentation
- Any thickening of the skin such as warts or skin tags
- Any ulcers or sores in the skin
- Any symptoms of persistent itching or soreness
Remember – skin cancer of the vulva is very rare, but to be certain, report all changes to your doctor.
Getting help
For immediate help, contact your local GP who should at least examine you and treat appropriately. Sometimes he or she will refer you to a hospital specialist such as a gynaecologist or dermatologist. If you have difficulty in getting help from your GP then you can go to a genitourinary medicine (GUM) clinic in your local hospital. Some hospitals have clinics dedicated to looking after vulval problems, but you will have to ask your GP.
Disclaimer
Nothing on this site is meant to qualify as a medical diagnosis. You should consult your doctor or other medical practitioner for a diagnosis and further information.